
The Therapist Is a Catalyst: Why Contextual Factors Will Transform Your Practice – Part 2 of 5
In our first post of this five-part series (read here!), we explored how the patient—through their beliefs, expectations, emotions, and readiness—acts as a primary contextual factor that influences every aspect of care. Now we turn the lens inward to examine a second crucial factor in clinical outcomes: the therapist.
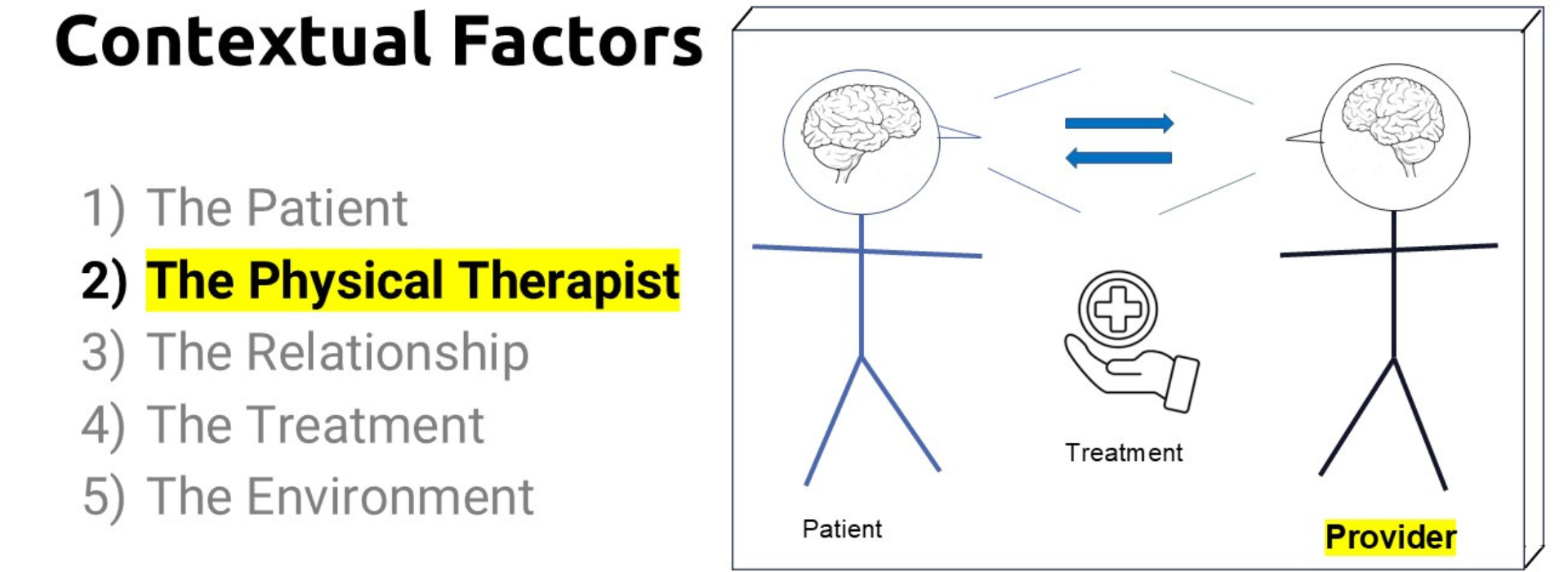
While it may be tempting to view ourselves as neutral agents delivering care, research tells a different story. We (as the healthcare provider) are not separate from the therapeutic process, we are deeply embedded within it. Who we are, what we believe, how we communicate, and the presence we bring into the room all directly shape the patient experience and influence recovery.
The Therapist as a Contextual Factor
Rossettini and other scholars in the growing body of literature on contextual factors [1,2] have identified the therapist as a powerful contributor to patient outcomes. The therapist's influence extends far beyond technical skill. Indeed, even the most evidence-based interventions can be amplified—or undermined—by how they are delivered.
Think about the times you felt most confident and connected with a patient. Chances are, those interactions went better.
Now, think of a time when you felt rushed, distracted, or uncertain. It likely showed, and the treatment experience likely suffered.
This isn’t anecdotal—it’s biological. Patients are finely tuned to our nonverbal cues. Mirror neuron system, affective attunement, and the co-regulation of emotional states all suggest that “how we show up” matters just as much as what we do.
Therapist-Driven Factors That Shape Outcomes
Let’s unpack what makes the therapist a contextual factor in clinical care:
1. Confidence and Credibility
Patients are more likely to engage with and benefit from care when they perceive their therapist as confident and competent. Confidence doesn’t mean arrogance, it means clear, grounded communication and assurance in your clinical reasoning. This can increase patient trust, adherence, and even reduce their perception of pain [3].
2. Communication Style
The words we use and the way we deliver them carry enormous weight. Therapeutic language that emphasizes safety, opportunity, and empowerment can shape beliefs and expectations. On the flip side, language that centers pathology, fear, or limitation can reinforce maladaptive narratives and nocebo responses [4].
3. Body Language and Presence
Patients notice more than we realize: posture, tone, eye contact, facial expressions, and timing. A therapist who is present and engaged creates a therapeutic atmosphere of safety and connection. This presence supports nervous system regulation and strengthens the therapeutic alliance [5,6].
4. Attitudes and Beliefs
What we know and believe about pain mechanisms, recovery, and the patient’s capacity to heal influences how we approach care. Therapists who are reflective of their own beliefs and adopt a biopsychosocial model and maintain a growth-oriented mindset are more likely to inspire confidence and autonomy in their patients [7].
5. Self-Awareness and Reflexivity
Perhaps most importantly, therapists must cultivate self-awareness. Our own stress, biases, assumptions, and emotional states inevitably shape our clinical interactions. Developing a practice of reflection—formally or informally—allows us to recognize our influence and adjust accordingly [8].
The Therapist’s Role in the Contextual Framework
Unlike the patient, who acts as the central processor of all therapeutic experiences, the therapist is the active shaper of that experience. We are meaning-makers, emotional co-regulators, and guides. We help the patient make sense of their symptoms and help them write a new narrative of recovery.
In this way, the therapist is unique among contextual factors. While the environment and treatment are relatively static, the therapist is dynamic, constantly interacting, adjusting, and responding. This responsiveness is both a responsibility and an opportunity.
A Real-World Illustration
Let’s return to our earlier example of a patient with chronic low back pain. Imagine two therapists:
- Therapist A provides detailed biomechanical explanations, emphasizes structural degeneration, and maintains a formal, distant demeanor.
- Therapist B frames degeneration as a normal part of aging, emphasizes movement as safe and beneficial, and communicates warmth, encouragement, and belief in the patient’s capacity to improve.
Both may prescribe the same exercise program. But the outcomes? Very likely different.
Therapist B has shaped the patient’s understanding, influenced their emotional state, and fostered a sense of safety and agency. The exercises are the same—but the context is transformed.
How to Cultivate Therapeutic Impact as a Contextual Factor
You don’t need to become a different person to have a meaningful impact—you need to become a more aware and intentional version of yourself in clinical practice. Here are a few strategies:
- Engage in self-reflection: Take five minutes after a session to consider how your communication, presence, and demeanor may have influenced the encounter.
- Use affirming, empowering language: Choose words that support autonomy and possibility.
- Practice state management: Your emotional regulation influences the therapeutic environment. Use mindfulness, breathing, or transition rituals to bring a grounded presence.
- Seek feedback: Consider using patient-reported experience measures to understand how patients perceive your engagement and effectiveness.
- Stay curious: Maintain a learner’s mindset. Seek continuing education in communication, motivational interviewing, and psychologically informed care.
What’s Next in the Series
So far, we’ve explored the patient and therapist as contextual factors—two dynamic agents at the heart of every therapeutic interaction. Next, we will explore the therapeutic relationship, the co-created space between patient and therapist that provides the foundation for trust, collaboration, and meaningful change.
Each remaining post in this series will continue to offer practical strategies, research-based insights, and real-world scenarios to help you apply the science of contextual factors in your everyday work.
Reflect on the following:
- How do I intentionally shape the “experience” of care?
How do you show up in the room? - Am I aware of the verbal and non-verbal messages I am sending
- In what ways can I adjust my beliefs and skills to be a more active part of the treatment?
- How am I influencing the patient’s belief in their ability to improve?
- What impact do you have on your patients beyond the techniques you deliver?
- What small shift in communication, presence, or mindset could make a big difference?
Remember: You are not a neutral party in the healing process. You are a powerful contextual factor. The way you think, speak, and connect is not an accessory to treatment—it is treatment.
Stay tuned as we move into the next layer of influence: the therapeutic relationship.
Looking for More?
This blog series is just a small window into the larger framework we teach inside our full course at Patient Success Systems.
If you’re finding this content useful, the course offers a deeper, more structured path. We explore the science behind contextual factors, break down communication strategies, and provide practical tools you can use to improve outcomes—day in and day out.
Whether you're new to these ideas or ready to refine your skills, the course is designed to meet you where you are and support your growth as a clinician who leads with thoughtfulness and precision.
👉 Learn more about the full course here.
Because when you strengthen the context around care, everything changes.
- Rossettini, G., Camerone, E. M., Carlino, E., Benedetti, F., & Testa, M. (2020). Context matters: the psychoneurobiological determinants of placebo, nocebo and context-related effects in physiotherapy. Archives of Physiotherapy, 10, 1-12.
- Poulter, D., Palese, A., Rodeghiero, L., Carlino, E., Esteves, J. E., Cook, C., & Rossettini, G. (2025). Contextual effects in musculoskeletal pain: are we overlooking essential factors?. Frontiers in Psychology, 16, 1537242.
- Day, M. A., Ehde, D. M., Sterling, M., & Jensen, M. P. (2025). How therapist effects shape pain-related outcome improvement in psychological treatments for chronic pain. Current Opinion in Psychology, 101995.
- Bedell, S. E., Graboys, T. B., Bedell, E., & Lown, B. (2004). Words that harm, words that heal. Archives of Internal Medicine, 164(13), 1365-1368.
- Arrigoni, A., Rossettini, G., Palese, A., Thacker, M., & Esteves, J. E. (2024). Exploring the role of therapeutic alliance and biobehavioural synchrony in musculoskeletal care: Insights from a qualitative study. Musculoskeletal Science and Practice, 73, 103164.
- Goldstein, P., Losin, E. A. R., Anderson, S. R., Schelkun, V. R., & Wager, T. D. (2020). Clinician-patient movement synchrony mediates social group effects on interpersonal trust and perceived pain. The journal of pain, 21(11-12), 1160-1174.
- Sherriff, B., Clark, C., Killingback, C., & Newell, D. (2023). Musculoskeletal practitioners’ perceptions of contextual factors that may influence chronic low back pain outcomes: a modified Delphi study. Chiropractic & Manual Therapies, 31(1), 12.
- Peterson, S., Miciak, M., Kleiner, M., Woolf, J., & Davenport, T. (2023). Drawing a “Perfect Circle”: How Clinicians Can Become Better Communicators. journal of orthopaedic & sports physical therapy, 53(10), 579-584.
Join Patient Success Systems!
Simply sign up below to get the latest delivered to your inbox.


